In each warm body it infects, the virus behind Covid-19 has the potential to change. It can become more deadly, more transmissible or more resistant to the vaccines on which we are all pinning so much hope. Mercifully, the biology of Sars-CoV-2 means that such changes happen slowly and almost always fail to catch on.
But mutations, like pandemics, are a numbers game. Every new person infected provides another opportunity for the virus to adopt a new form. So far, Sars-CoV-2 has infected at least 106 million people worldwide and taken on many thousands of mutations. Most of those changes are slow and inconsequential – evolutionary dead ends that nobody will ever realise existed. But, in some people, the virus hits the jackpot.
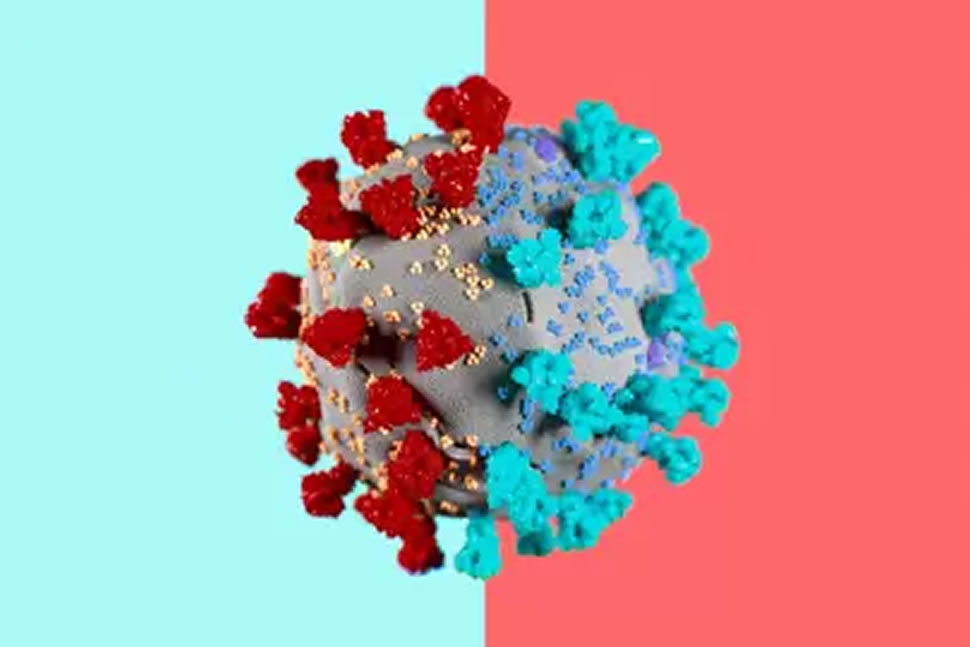
That is seemingly what happened in Kent in September 2020. Usually Sars-CoV-2 mutates slowly. We can watch this happen, with single letters changing one at a time in a viral genome that contains almost 30,000 letters. But, in one great leap, the UK variant picked up 17 of those changes. Eight of them happened in the gene that encodes the spike protein – the hook the virus uses to latch on to and enter human cells. If the genome of Sars-CoV-2 was a 30,000-character-long poem then the UK variant re-wrote its first line, drastically changing its meaning in the process.
The emergence of the UK variant presented scientists with an urgent question: how did the virus make this genetic leap, seemingly out of nowhere? The leading hypothesis is that the new variant evolved within just one person, infected with Sars-CoV-2 virus for so long that the virus was able to evolve into a new, more infectious, form. Out of this human pressure cooker, a new variant burst onto the scene and sent the world scrambling to react. Borders closed, countries locked down once more, vaccines were re-tested.
None of this was enough to halt the spread of B.1.1.7 – the scientific name given to the UK variant. The new variant has now been found in 75 countries and is spreading locally in Brazil, Canada, China, the United States and most of Europe. Up to 70 per cent more transmissible than other coronavirus variants, B.1.1.7 is now responsible for the vast majority of new cases in England. On January 22, the UK’s chief scientific officer, Patrick Vallance, added another worry to the list: preliminary data suggests that the new variant may be 30 per cent more deadly than others.
Chronic infections are rare events, but give a virus enough hosts to infect, and these rare events are almost certain to happen. Now, as worrying new variants spread in other parts of the world, scientists are racing to understand the role that chronic infections might play in the emergence of new variants, and how to stop the next one before it takes hold.
Sars-CoV-2 may be the most surveilled virus in history. In the 13 months since virologists Zhang Yongzhen and Edward Holmes published the entire genome of the virus, more than 360,000 Sars-Cov-2 genomes have been sequenced and uploaded to GISAID – a platform for sharing viral genomes. Almost half of those genomes came from the UK, which sequences roughly ten per cent of all its positive Covid-19 tests, making the country a canary in the coal mine for detecting new variants.
As B.1.1.7 has shown, the speed at which variants are detected will be key in the next phase of the pandemic, but genomic surveillance only gives us a partial picture of how a virus is changing. The first example of the UK variant was found on September 20 in Kent and then another one day later, in a sample from Greater London. On its own, the appearance of a new variant in genomic databases doesn’t tell us much about where the virus is heading. “That’s just one genome amongst thousands every week. It wouldn’t necessarily stick out,” says Oliver Pybus, a professor of evolution and infectious disease at the University of Oxford. New variants of Sars-CoV-2 are being created all the time but the vast majority of them go absolutely nowhere.
It was only when it became obvious that lockdown measures in Kent were failing that Public Health England (PHE) realised the outbreak was being driven by a new variant. By the first week of December, it was clear that the new variant was rapidly becoming the dominant variant in certain parts of the UK. Of the 915 cases of the new variant identified in Public Health England’s initial report on the outbreak, four dated from September and 79 were recorded in October. In November there were 828. Data from positive cases gave health authorities an important clue about the new variant’s behaviour: it seemed to be transmitting more readily than existing variants. But the data couldn’t explain where the new variant had come from. The emergence of the UK variant, with its 17 significant genetic changes, seemed to defy the logic of what we know about how coronaviruses evolve.
In evolutionary terms, Sars-CoV-2 is a genetic slowpoke. Viruses mutate as they pick up tiny errors in their genetic code when they make copies of themselves, but coronaviruses have evolved an extra trick that makes this copying process more accurate. Coronaviruses have proteins that spot and correct mistakes in their RNA, which slows down the number of errors that accumulate in their genome. Sars-CoV-2 tends to pick up one or two mutations per month – slower than flu or polio but faster than measles. “It was unusual in September to all of a sudden see [a variant] pop up that had 17 [changes],” says Adam Lauring, an associate professor at University of Michigan Medical School who studies the evolution of RNA viruses like Sars-CoV-2. “It suggested that something unusual happened.”
The odds are stacked against any one mutation taking hold and becoming the dominant strain in an outbreak. Although the Sars-CoV-2 virus starts replicating within days of infecting a person, producing lots of genetically distinct viruses as it does so, most of these mutants never grow to make up a significant share of all the Sars-CoV-2 viruses within a host. “Most of them are dead-enders,” says Lauring. “They go nowhere. They die within a person and we never find out about them.”
When viruses do mutate, they tend to pick up changes slowly enough that genetic epidemiologists can see the emergence of a new strain in real-time. The distinctiveness of the UK variant pointed to two likely origin stories: either the virus had mutated abroad and only been detected once it entered the UK, or many of the changes had happened within one person. Since most countries don’t have high levels of genomic surveillance like in the UK, it’s impossible to know conclusively whether the variant originated in Kent, or was just detected there for the first time. But most countries affected by the new variant have strong travel links with the UK, suggesting that it is the country of origin, says Pybus.
A third possibility is that the variant emerged through something called recombination. Viruses can sometimes swap parts of their genome with other viruses from similar strains, bringing in a set of mutations all in one go. But, again, evolutionary biologists haven’t seen any evidence of ancestor strains in the UK that may have blended together to create the UK variant. This leaves one remaining likely hypothesis: the UK variant emerged from just one person.
For most people who get infected, Covid-19 lasts two weeks. People with mild cases usually test negative for the virus ten days after first showing symptoms. In more severe cases, people can continue to spread the virus for up to 20 days after their first symptoms. For an unlucky subset of patients Covid-19 infections last much, much longer.
There are multiple documented cases of patients with chronic Covid-19 infections that last several months or more. With his colleagues at the University of Michigan, Lauring documented the infection of one man who had harboured the replicating virus for at least 119 days. By analysing the genomes of virus samples taken at different points during the patient’s infection, Lauring could see the virus steadily accumulating genetic changes – a microcosm of how Sars-CoV2-2 mutates within the global population, but this time all happening within one human host.
Sars-CoV-2 isn’t the only virus that can linger for an unusually long time within the human body. Ebola virus RNA has been detected in the semen of men a year after they recovered from the virus. Some people stay infected with norovirus – a common stomach bug that causes vomiting and diarrhoea – for more than six months. One man in the UK has excreted infectious poliovirus for at least 28 years. The man had been shedding mutated virus for so long that researchers writing about his infection said that he, and other chronic excretors, pose an “obvious risk to the [polio] eradication programme”.
Those who become chronically infected tend to have something in common: their immune systems are compromised in some way that makes it impossible for them to fully get rid of an infection. The man Lauring studied was undergoing chemotherapy for cancer of the lymph nodes, which likely hampered the production of immune cells that respond to new viruses. The man who shed poliovirus for at least 28 years suffered from a disorder called common variable immune deficiency, which decreases the number of antibodies in the blood and makes it harder for the body to fight off infections.
People with weakened immune systems provide viruses like Sars-CoV-2 with a unique environment. Instead of clearing an infection quickly, an immunocompromised person might only partially wipe out an infection, leaving behind a population of genetically-hardier viruses that rebound and begin the cycle all over again. In these people, a virus can evolve at remarkable speed. “The whole time, their immune system is effectively beating [the virus] up. So the virus has a chance to learn how to live with the human immune system,” says Emma Hodcroft, a postdoctoral research at the University of Bern in Switzerland who works on Nextstrain – an open-source project that tracks the genetic changes of Sars-CoV-2 and other pathogens.
This is similar to what’s happening on a global scale. Slowly, natural selection might push the virus to transmit more easily, or become resistant to our immune response, but in the pressure-cooker environment of a single human body these changes can accelerate. Ravi Gupta, a professor of clinical microbiology at the University of Cambridge studied the evolution of Sars-CoV-2 in a man with lymphoma who had undergone chemotherapy and had been chronically infected with the virus for 102 days before dying.
After the man was treated with blood plasma from a recovered Covid-19 patient, at day 63 of his illness, the genetic makeup of the Sars-CoV-2 viruses within him started to shift. By day 82, viruses with a six-letter deletion in the spike gene were now the dominant population. This deletion – called ΔH69/V70Δ – also seems to be partly behind the increased transmission of the B.1.1.7 variant, as it makes it easier for the virus to enter host cells. The same mutation was also found in another chronically infected patient, a 47-year-old woman admitted to hospital in Saint Petersburg who has been ill for more than four months.
Within the man Gupta and his colleagues studied, the composition of the viral population kept changing. By day 86, the ΔH69/V70Δ population had been overtaken by a subset of Sars-CoV-2 with a different mutation in its spike gene. A week later both of these previous populations were barely anywhere to be seen and a new mutant had become the most populous strain.
For Gupta, this genetic tug-of-war is a likely explanation for the emergence of the UK variant. “What’s going on biologically within a person is probably going to explain this because there are very different selection pressures going on,” he says. Since Sars-CoV-2 infects cells relatively quickly, in most cases it enters a host, replicates and then swiftly infects someone else, leaving little time for the virus to acquire many genetic changes. When the virus enters the body of someone who is already immunocompromised, their body is constantly applying evolutionary pressure on the virus – pushing it to evolve into new and, in some cases, more infectious forms.
We may never know for sure how the UK variant emerged but we could be doing more to track and understand how the virus mutates within chronically ill people. “In an ideal world we would know who’s shedding virus for long periods of time and we would be able to sequence them to check what’s happening,” says Gupta. It might mean limiting the use of convalescent plasma – which in Gupta’s study appeared to push the virus to acquire mutations – to cases where severely immunosuppressed patients could be isolated and monitored.
But the real problem isn’t chronic infection – it’s a situation where the pandemic is so out of control that the virus has endless opportunities to mutate into new variants. That situation is a reality in the UK and in dozens of other countries with dangerously high case rates. “These are all edge cases, but if you have enough people infected over a long time, you run the risk of hitting those edge cases,” says Hodcroft. It is not surprising that some of the most worrying new variants – from Brazil, South Africa and the UK – emerged from parts of the world with relatively high levels of transmission. “When you have millions of people infected, with millions of viruses replicating in each one, there are lots of chances for the virus to explore new mutations and combinations,” says Lauring. “If we had control of the virus, we wouldn’t be seeing as many variants pop up, because there wouldn’t be as many opportunities for evolution to happen.”
Stopping the emergence of new variants means doing more of what we know stops transmission: wearing face masks, social distancing, working from home and tracing infections. Although data from Israel shows that vaccines are a powerful tool for stopping hospitalisations and infections, alone they are no defence against the emergence of new variants. Epidemiologists fear that a combination of widespread transmission and a partially-vaccinated population might push Sars-CoV-2 to acquire vaccine-evading mutations.
One thing we do have on our side is genomic sequencing. Within weeks of the UK variant being observed, Gupta and his colleagues were able to show how its genetic changes caused it to become more infectious by attaching its spike protein to HIV particles. They could then measure how successfully the modified viruses were infecting human cells. Trials to test how well vaccines protect against new variants have also been releasing results at breakneck speed. “That’s mind-boggling compared to the speed at which science moves in ordinary circumstances,” says Jeffery Barrett, director of the Covid-19 Genomics Initiative at the Wellcome Sanger Institute.
In mid-January, genomic surveillance picked up another worrying mutation in some of the UK variant viruses: a change called E484K, also present in the South Africa variant, that helps the virus evade the body’s immune system. As our immunity to Sars-CoV-2 grows through vaccines and infection, the virus is pushed to find new adaptations that allow it to continue infecting and spreading. We are watching the virus evolve in real-time, but watching is not enough. “We can’t afford to keep giving the virus more and more chances to mutate to new, stable configurations,” says Barrett. “Keeping the current restrictions until we really get transmission down is very, very important.”
This article originally appeared on wired.co.uk
All the latest Business News brought to you by AIM Internet.
AIM Internet specialise in digital marketing services that provide strategic online marketing solutions to grow your business. Contact us today to find out more.